Ask around in almost any primary care setting or hospital corridor these days, and you’ll hear the same. Doctors and nurses are wondering if it’s time to pack in the NHS and try their hand at private practice.
And it’s not surprising.
Long hours, endless and tedious admin work, and the guilt of rushing through patients in ten minutes flat all contribute to burnout and low job satisfaction.
It takes a serious toll on people’s mental health and overall well-being, leaving many frustrated, exhausted, and quietly craving a way to practice medicine on their own terms.
Therefore, in this blog, we’ll explore this topic and explain how you can transition from NHS employment to private medical practice.
Why GPs consider leaving the NHS
The simple answer to this is that the workload in the NHS has ballooned, while resources have shrunk.
GPs talk about:
- 12-hour days that still don’t feel enough
- Unmanageable ten-minute appointments and rigid targets
- The constant sense of being behind
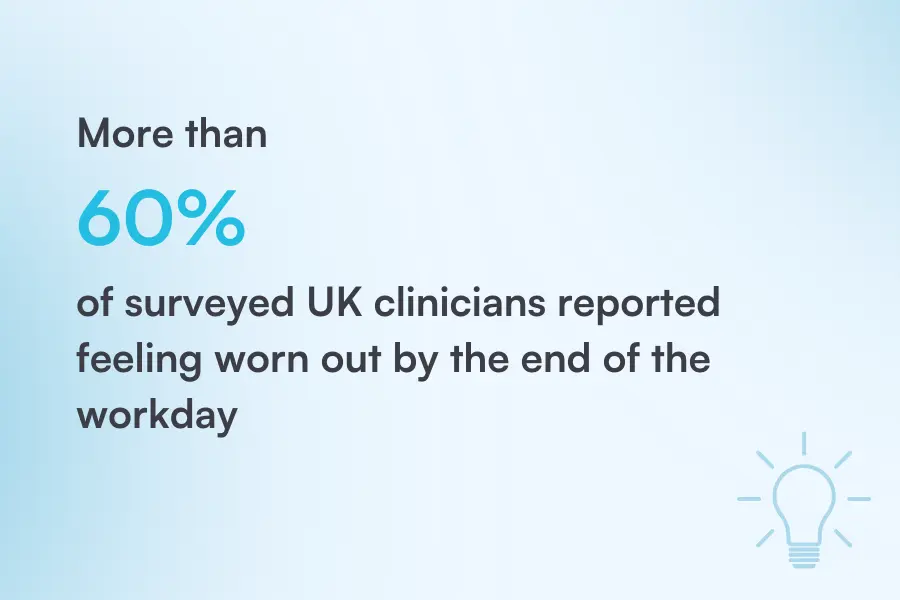
Illustration: Pabau / Data: Bain & Company
In addition, the system itself doesn’t help, leaving healthcare professionals at a breaking point, with many planning to reduce their hours or quit altogether.
On the other hand, NHS patients are growing increasingly frustrated with waiting weeks for appointments and are willing to pay for quicker access.
For doctors, this demand is fueling the opportunities for growth in the private sector, making private healthcare more viable than ever, offering a better work-life balance and stronger earning potential.
How does transitioning from the NHS to private practice affect a doctor’s career?
The move from NHS to private practice isn’t just a change of scenery, it reshapes a doctor’s whole career.
Here are the key aspects that affect a doctor’s career when it comes to transitioning from the NHS to private practice:
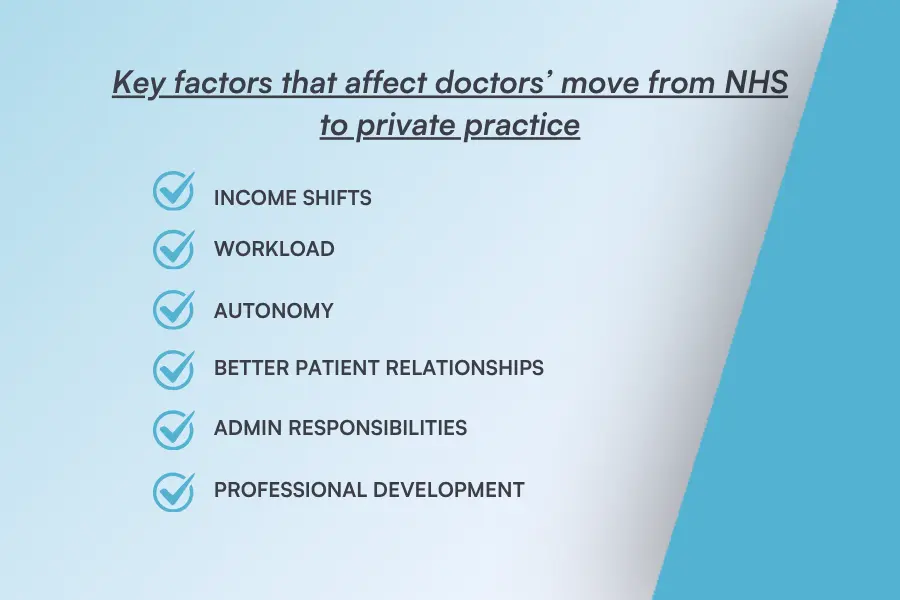
Source: Pabau
- Income shifts: Earnings are tied to patient volume, services offered, and often business
- Workload: The hours can be more flexible; you may see fewer patients in a day, but spend more time on non-clinical work
- Autonomy: Doctors often have more say in how they practice, which treatments they offer, and how their clinic operates
- Better patient relationships: With longer appointment times and less pressure to rush with patients
- Admin responsibilities: Taking on tasks like compliance, payroll, and marketing
- Professional development: Doctors get more flexibility for specialization and expand the health services
In short, those who leap often find more freedom and better pay, but they also discover that the trade-off is taking ownership of every aspect of their practice.
Start your own vs. join an existing practice.
One of the most significant decisions NHS staff may face throughout their careers is whether to enter the private sector. The typical options for this are:
- Start their own clinical practice: Have full control, choose the location, branding, services, and setup, but also have full responsibility and face hefty startup costs
- Buy into a partnership: Gain a stake in an existing clinic, with all the infrastructure already in place, but you’ll have less control over decisions
- Join an existing healthcare provider: You won’t have to worry about handling the admin, marketing, and facilities, but at the same time, you don’t have full autonomy
Bottom line: if you want independence and have capital, start your own practice. If you prefer easing into ownership without the stress, join an existing setup.
Steps for transitioning from NHS to private practice as a healthcare professional
The leap from the NHS to private practice starts with you handing in your notice. But it doesn’t end there, it’s a process.
Let’s take a look at the key steps to take to make the transition.
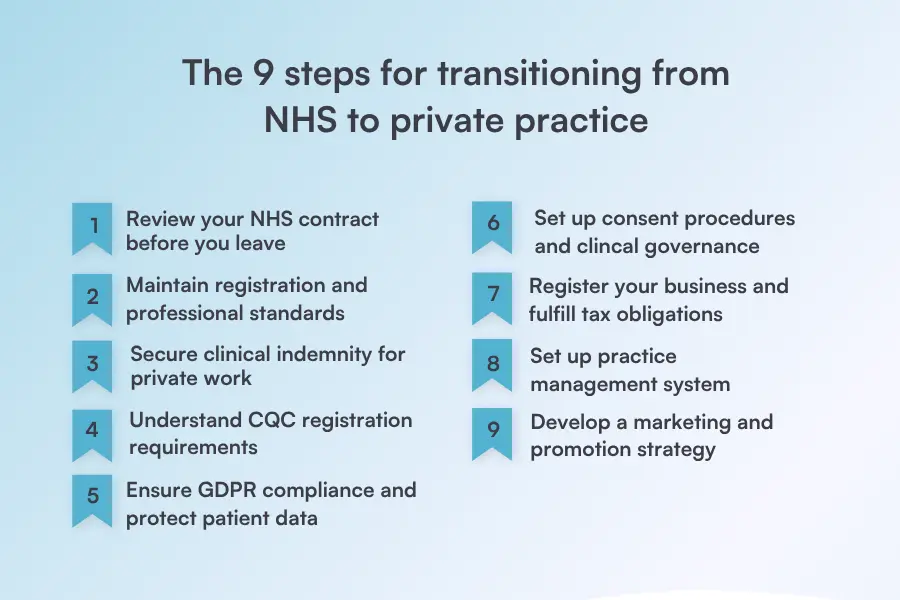
Source: Pabau
1. Review your NHS contract before you leave
Before making any moves, dig out your NHS contract. This is crucial because many contracts have:
- Specific notice periods you need to give
- Rules about secondary employment
- Clauses designed to prevent conflicts of interest
Also, ensure that your private work doesn’t interfere with your NHS duties, including the use of NHS resources such as staff, equipment, patient lists, or your NHS email for private purposes.
Failing to address these issues can lead to disciplinary problems or even legal consequences.
2. Maintain registration and professional standards
Leaving the NHS doesn’t mean leaving the rules behind. Also, patients don’t care whether you’re NHS or private. They expect the same standards of professionalism and safety.
You still need to be registered with your regulator and continue fulfilling appraisal and revalidation requirements, whether that’s the:
- General Medical Council (GMC)
- Nursing and Midwifery Council (NMC)
- Health and Care Professionals Council (HCPC)
Keeping your registration up to date ensures your practice is beyond reproach.
3. Secure appropriate clinical indemnity for private work
The moment you start seeing patients in your private practice, you need your own professional indemnity.
Providers like the Medical Defense Union MDU or the Medical Protection Society (MPS) specialize in this, offering coverage tailored to private practice risks. This includes:
- Protection against clinical negligence claims, including legal defense and compensation
- Support for disciplinary proceedings
- Assistance with coroners’ inquests
- Legal advice and representation for professional matters
- Coverage for emergency care abroad
- Run-off cover after retirement to handle past claims
Think of this as your safety net so you can practice without constantly worrying about ‘what if’.
4. Understand CQC registration requirements
In the UK, private practices must understand CQC requirements and it’s role and must also register with it before they begin treating patients. The CQC will check if the services you intend to offer meet the safety, quality, and governance standards.
If your private practice is based in Scotland, Wales, or Northern Ireland, the regulatory bodies for this type of registration are different, for example:
Although these regulatory bodies may have slightly different registration requirements, their core principles remain the same, and understanding how to navigate investigations into violations is crucial.
5. Ensure GDPR compliance and protect patient data
Private or NHS, patient confidentiality is non-negotiable.
In private practice, you’re personally responsible for GDPR compliance. This involves registering with the Information Commissioner’s Office (ICO) and implementing data protection policies to ensure that personal health information can be managed safely and securely.
Also, this includes:
- Storing patient records securely
- Controlling who has access to what information
- Ensuring all staff members understand confidentiality obligations
- Setting clear policies for handling, sharing, and disposing of patient data to help prevent breaches and uphold ethical standards
At the end, it’s all about trust. Patients need to know their data is safe with you. Also, you don’t want a breach that could destroy your reputation overnight.
6. Set up consent procedures and clinical governance
Unlike NHS consents, in private practice, they’re more than just a signature.
It’s crucial that patients complete them before appointments and truly understand the treatment they’re about to have, the treatment outcome, its risks and alternatives.
Source: Pabau
This means investing time in clear, jargon-free conversations, double-checking patient expectations, and documenting everything in writing to ensure accuracy. For this, digital consent forms can streamline the process and reduce the risk of missing details.
Beyond that, you’ll also need strong clinical governance to underpin the quality and safety of your service. At a minimum, you’ll need:
- Compliant handling protocols so issues are resolved fairly and transparently
- Risk management systems to identify and mitigate potential safety concerns before they escalate
- Incident reporting procedures that ensure accountability within the practice
These procedures mirror the standards regulators look for and reassure patients that your clinic runs to the same quality benchmarks as any hospital or NHS service.
7. Register your business and fulfill tax obligations
Once you start working privately, you won’t just be a doctor. You’ll also be a business owner, and this means:
- Deciding on the legal structure of your private practice as a business: A sole trader, a partnership, or a limited liability company
- Registering with His Majesty’s Revenue and Customs (HMRC): Filing annual returns, paying income tax or corporation tax, and keeping accurate financial records
- Conducting regular tax returns: If your turnover crosses the VAT threshold, you must also register for VAT
Also, if your private practice is a limited company, you must file annual accounts and confirmation statements with Companies House to maintain a public record of your business.
8. Set up practice management system
The reality is that managing a private practice with paper and spreadsheets leads to chaos.
To escape that, you’ll need a smart digital system from the start that keeps track of bookings, records, billing, communication, and everything else in order.
For example, a robust system like Pabau. It’s a robust software solution made for private healthcare practices in mind, with key features for GP practices, such as:
✅ Electronic medical records that capture essential patient medical history, questionnaires, and allergies to treatment notes
✅ Letter templates you can easily generate, personalize, and send to patients or third parties without the need to repeatedly type the same information
✅ Order and get lab results within Pabau through The Doctors’ Laboratory
✅ Comprehensive client records that store patients’ detailed medical history
✅ Centralized Prescriptions that allow you to create, send, and track all prescriptions from one place
✅ Client referrals to record referrals sent from external sources like the NHS, insurance programs, or healthcare partnerships
…so everything you need is at your fingertips, making day-to-day operations run smoother and stress-free.
9. Develop a marketing and promotion strategy
Patients won’t just find you. You need to go out there and get them, and usually that starts with having a professional website and a Google Business Profile, so you show up in local searches.
It’s important to:
- Run Google Ads to get quick traction
Another thing not to underestimate is the power of word of mouth and partnering with local gyms, wellness centers, or community groups. This can put you in front of your ideal patients.
Make a smooth transition to private practice with Pabau
Leaving the NHS can be tough, but it can also reignite your passion, improve your work-life balance, and give you more autonomy.
Nobody says transitioning to a private practice will be easy since you also need to step into the business side, but there are solutions to take the pressure off.
One such solution is Pabau. It’s all-in-one software handles appointments, patient records, billing, automated reminders, and marketing, reducing admin so you can focus on patients and growth.
It’s time you explore how Pabau can support you in making a smooth transition from the NHS to private practice and help you run a successful practice. Book a demo today and streamline your clinic with ease.