Put yourself in your patient’s shoes and ask yourself — what kind of care would you want to receive?
Let me guess — safe, caring, effective, and quality care, from a staff that is responsive to all your needs and preferences.
And who wouldn’t?
This is precisely what the Care Quality Commission (CQC) is all about — protecting patients by ensuring they receive the best possible care.
In England, registering with the CQC isn’t just a recommendation; it’s a legal requirement for all health and social care providers.
But if you work in aesthetics, it’s a bit of a gray area. For those transitioning from the NHS to private practice, knowing which treatments require CQC registration is crucial.
Whether you need to be registered or not depends on what treatments you offer, i.e. surgical cosmetic procedures versus non-surgical aesthetic procedures. But you may be surprised by some treatments you need to be CQC registered for, such as IV drips and thread lifting.
That’s exactly why we compiled this blog, so you can get a clearer understanding of the Care Quality Commission, its role, and what you need to know as a practitioner.
What is the CQC (Care Quality Commission)?
Simply put, the CQC makes sure that health and social care providers deliver services to individuals that are safe, compassionate, responsive, effective, and well-led.
Almost all health and care service providers in England – hospitals, aesthetics practices, and even educational facilities that provide care for children, are obliged to register with the CQC.
Subsequently, the CQC oversees, inspects, and evaluates health care providers. If required, the CQC intervenes to improve or, in severe cases, shut down services that fall short of meeting the set standards, regulations, and legal requirements.
What’s important to know is that the CQC serves as the independent regulator for health and social care services only within England, not the UK.
What is the role of the CQC (Care Quality Commission)?
The CQC has a crucial role in making sure that all registered health and social care providers offer safe and top-quality care. Their role involves:
- Registering care providers and services
- Inspecting, monitoring, and rating the quality of the services
- Protecting the individuals who use these services
- Sharing their opinions and views on the quality issues of the services in health and social care
Another role of the CQC is to provide the public access to their inspection reports. This will help people make informed decisions when choosing the best care for themselves, a family member, or a friend.
What are the Care Quality Commission (CQC) fundamental standards?
The fundamental standards are the minimum requirements a healthcare provider must meet when providing care to patients.
There are 13 fundamental standards:
1. Person-centered care — Each person’s care or treatment should be customized to suit their individual needs and preferences.
2. Dignity and respect — Everyone who receives care should be treated with dignity and respect, and healthcare providers must make sure the patients are:
- Given privacy whenever they need or want
- Treated as equals
- Given the support they need to help them remain independent and involved in their local community.
3. Consent — Before receiving any care or treatment, patients (or their legal representative) must provide consent.
4. Safety — Healthcare providers are responsible for evaluating potential risks to patient’s health and safety during any care or treatment. They must ensure their staff possesses the qualifications, competence, skills, and experience required to keep patients safe.
They shouldn’t receive care or treatment that is unsafe or places them at harm or risk that can be avoided.
5. Safeguarding from abuse — While receiving care, patients should not endure any kind of improper treatment or abuse. This includes:
- Demeaning treatment
- Neglect
- Use of unnecessary or excessive restraint
- Inappropriate restrictions on their freedom.
6. Food and drink — Patients must have enough to eat and drink while they receive treatment.
7. Premises and equipment — The locations and places where you provide care and treatment and the equipment you use must be suitable, clean, secure, used, and looked after properly.
8. Complaints — Patients have the right to express concerns about the care and treatment they receive, and the care provider must address and respond to the complaints. Care providers should investigate the situation and take appropriate action if they identify any issues.
9. Good governance — The care provider needs to have robust governance and systems in place to monitor the quality and safety of the care they provide. These systems should facilitate service improvement and mitigate any risks to your health, safety, and well-being.
10. Staffing — The care provider must have appropriately qualified, experienced, and competent staff to ensure they meet these CQC fundamental standards, which is why having structured LPN interview questions matters when you’re hiring.
11. Fit and proper staff — The care provider must hire individuals capable of delivering care and treatment suitable for their assigned roles. They should pass through professional recruitment procedures and conduct necessary background checks for applicants, such as assessments of work history and criminal record verification.
12. Duty of candour — The care provider is obligated to be honest and open with their patients regarding their care and treatment. In the event of an error, they must inform the patients about what happened and why, offer support, and issue an apology.
13. Display of ratings — The care provider must visibly present their CQC rating where it will be accessible to patients. Additionally, they are required to include this information on their website and provide access to the public to their most recent service report.
Which organizations are regulated by the CQC?
Organizations that need to register as Care Quality providers, and thus be regulated by the Care Quality Commission fall under these services:
- Clinics, including slimming and family planning clinics
- Doctors and dentists GPs, including general practices, out-of-hours services, and walk-in centers
- Mental health services
- Ambulances, both independent ambulance services and National Health Service ambulance services
- Independent hospitals and NHS (National Health Service) trusts
- Care homes, including nursing and residential homes
- Community-based services, including substance misuse services and services for people with learning disabilities
- Services over the phone, mobile doctors, and home care agencies
- Hospice services for people who are nearing the end of their lives or have life-limiting conditions
The CQC also collaborates with relevant authorities to conduct cross-sector inspections and oversee and regulate:
- Emergency and urgent care systems
- Children’s health services
- His Majesty’s Inspectorate of Prisons
- Defence medical treatment facilities
In summary, anyone who provides medical treatments, personal care, nursing care, or maternity and midwifery services must be registered and regulated by the CQC.
CQC and aesthetics clinics
Aesthetic clinics can perform a wide range of cosmetic procedures, from non-invasive procedures to surgeries and liposuction. By law, if your aesthetics clinic provides medical services like the ones listed below, then you must register with the CQC:
- Liposuction — including laser lipolysis
- Thread lifting — all types
- Cosmetic surgeries that involve inserting equipment or instruments into the body — including facelifts, breast surgery, brow or eyelid surgery, nose surgery, buttock or thigh lifts, tummy tucks, or any other procedure where an implant is used
- Lens implant surgery or refractive eye surgery
The CQC doesn’t regulate other procedures that aesthetics clinics provide. So, clinics that offer procedures like the ones listed below don’t need to register for CQC inspection.
- Subcutaneous injections, like chemical peels and dermal fillers
- Subcutaneous injections of muscle relaxants used to change the appearance, like anti-wrinkle treatments. It’s worth noting this this is only the case if Botox is being used purely cosmetic purposes. If it’s for a medical reasons, this is in scope.
- Intense pulse light (IPL) and laser treatments such as skin rejuvenation or hair removal
- Thread lifting performed by a beautician or someone who is not a healthcare professional.
- Cosmetic procedures that involve inserting or cutting equipment or instruments into the body — like facelifts, buttock or thigh lifts, and tummy tucks — that are performed by someone who is not a registered healthcare professional.
While some of these examples seem quite surprising – how can someone who isn’t qualified as a healthcare professional carry out a surgical procedure such as a tummy tuck without needing to be registered, for example? – we don’t make the rules unfortunately.
This also may be why the industry as a whole is reviewing current licensing practices…
New licensing regulations
Poorly performed aesthetic procedures, unfortunately, can leave people mentally and physically scarred. To prevent the risk associated with ineffectively performed non-surgical cosmetic procedures and to improve overall standards, the UK Government has introduced a new licensing scheme with the new Health and Care Act 2022.
This new legislation will apply to those who perform derma fillers, antiwrinkle treatments, and any other procedure that penetrates the skin or under or uses light, electricity, cold, or heat.
The new licensing scheme will apply to practitioners and premises where the treatments are performed.
Practitioners — The regulations will prohibit individuals in England from performing specific cosmetic procedures as part of their business activities unless they possess a valid personal license.
Premises — With this regulation, individuals will be restricted from using or allowing the use of premises in England for conducting specified cosmetic procedures as part of their business activities unless they hold a valid premises license.
These regulations are new and still not applicable, (and might not be until 2026) it’s always good to be prepared in advance.
While this doesn’t relate to CQC specifically, it’s something to be aware of if you’re in the industry or looking to open your own practice in the future.
Why is CQC important for my medical practice?
CQC will ensure patient safety
The primary goal of the CQC is to guarantee the safety and effectiveness of health and social care services for patients. Adhering to CQC standards helps businesses ensure the delivery of safe care and reduce potential harm to patients. The focus on safety can contribute to increased patient satisfaction and better patient outcomes.
Complying with CQC regulations is a legal obligation
Non-compliance with the CQC regulations and standards may lead to penalties or, in severe cases, shutting down of the healthcare business. By following the CQC requirements, healthcare businesses can steer clear of legal consequences and guarantee that they meet the necessary care standards.
Improving staff satisfaction
Complying with CQC standards not only covers crucial aspects for patients but for staff members too. This includes having adequate staffing levels, providing training, and supporting the staff’s well-being. When complying with these regulations, healthcare businesses can ensure that their staff receive the necessary resources to deliver high-quality care. This support can reduce staff turnover and boost morale.
Quality assurance
Adhering to CQC requirements can help healthcare businesses maintain high-quality care standards when providing their services. Compliance with CQC ensures the implementation of effective quality assurance processes — keeping an eye on proper staff training and keeping accurate and updated records at all times.
Building reputation
Healthcare businesses that receive a good rating from the Care Quality Commission after inspection are more likely to be trusted by patients. Receiving a good rating helps healthcare businesses attract new patients and build a shining reputation. Patients often use the CQC rating system as a starting point to make an informed decision about which service provider they’ll go to.
CQC inspection
Facing a CQC inspection can feel the same as taking a test — even if you know everything, there’s still a sense of being overwhelmed and under pressure.
However, as the saying goes, it’s better to be safe than sorry. That’s why being thoroughly prepared when CQC inspectors arrive is crucial.
Here’s what you need to know about the inspection process.
The CQC inspection is divided into three departments:
- Departments that inspect hospitals
- Departments that inspect general practices (including medi aesthetic clinics)
- Departments that inspect adult social care
A Chief Inspector is responsible for leading the inspection team, which consists of physicians, general practitioners, nurses, social workers, and members of the public.
The process:
Step 1: The start of the visit
A senior member of the organization will typically be approached by the CQC inspector or inspection team to discuss the inspection’s goals and objectives, staff, and the method of how they will present the results.
Step 2: Collecting evidence
Through comment cards, complaints, group or one-on-one interviews, and pop-up engagement stalls, the CQC team will gather feedback from patients who reside in the healthcare organization that is inspected.
The team will also observe how and where the treatment is provided to patients, and the patient journey, and review the practice’s records, policies, and documents.
Step 3: Providing feedback
At this last stage, the Chief inspector or a senior staff member of the inspection team will present the findings they gathered during the inspection process and share their feedback with a senior member of the healthcare practice.
They will give an overview of their conclusions, draw attention to any problems that require fixing, list any particular steps that the healthcare organization needs to take right away, describe the process by which they will make their judgments and share them with the public, and discuss their upcoming visit.
The 5 questions CQC inspectors follow when evaluating services
The 5 CQC questions or 5 KLOE — key lines of enquiry (also known as the 5 CQC domains, or 5 CQC standards) were drawn out of the fundamental standards we’ve discussed above.
These 5 CQC questions help the ones doing the inspection focus on the things that matter most to people.
Here’s what the inspectors ask themselves when they evaluate the services:
- Are they safe?
Are patients, visitors, and staff protected from avoidable harm and abuse?
- Are they effective?
Does the care, support, and treatment you’ll provide be evidence-based and will lead to positive results, and improved quality of life?
- Are they caring?
Does the staff treat and involve patients with kindness, respect, compassion, and dignity?
- Are they responsive to the patient’s needs?
Are services organized in a way to meet patient’s needs?
- Are they well-led?
Does the management, governance, and leadership of the healthcare organization ensure that the care provided is of high quality and based on the patient’s individual needs, fosters innovation and learning, and advocates for a fair and open culture?
Types of CQC inspection
There are 2 types of inspection. Comprehensive and focused.
Comprehensive:
A comprehensive inspection is where the CQC inspects all the healthcare provider’s services based on the 5 key CQC questions and rates them on a four-point scale.
The comprehensive inspection is announced in advance, with a minimum of two weeks’ notice. The duration of the inspection usually lasts less than a day, but it may be extended based on the scale and nature of the services that are under review.
Focused:
While the focused is usually announced, the CQC may also carry out an unannounced inspection, for instance, if they are responding to a particular concern or issue.
The focused inspection doesn’t review all of your services, but the process is very similar to the one for comprehensive inspections. The biggest difference is that the inspection team does not follow all 5 key questions.
Focused inspections serve two primary purposes — to address a specific concern or to follow up if some changes were made.
CQC ratings
There are four ratings that the CQC gives to the healthcare services they inspect: inadequate, requires improvement, good, and outstanding.
| Inadequate | The service is underperforming, and the CQC will implement corrective actions against the responsible organization or individual. |
| Requires improvement | The service is not meeting expected performance levels, and the CQC will communicate the specific areas for improvement that are required. |
| Good | The service meets the CQC expectations and is performing well. |
| Outstanding | The service performs exceptionally well. |
The ratings that the CQC gives the healthcare provider must be transparent to the public. You are legally required to display the ratings given by the CQC in the places where you provide services. This could include the primary entrance of a healthcare organization, the waiting area, or even the business website.
Inspection frequency
The frequency of the inspection depends on the previous ratings the healthcare organization has received from the CQC.
So, if the healthcare business has an inadequate rating, then the maximum time between inspections will be six months.
If the services require improvement, then the time between inspections will be one year.
For the healthcare practices that have good or outstanding ratings, the inspections will be performed every five years.
How can medical practices prepare for a CQC inspection?
Step 1: Familiarizing with the inspection process
Medical businesses should learn the whole process and what inspectors look for when they do the inspection, so they can understand what is expected of them.
Step 2: Creating internal audits
Regular internal audits are crucial for businesses to pinpoint areas that need improvement and to guarantee compliance with CQC regulations and standards. These audits should include training, staffing, record-keeping, governance, and quality assurance.
Step 3: Create action plans
After pinpointing the areas that need improvement, businesses should create action plans to tackle these issues. These plans need consistent review and updates to track and ensure ongoing progress.
Step 4: Staff training
All staff must receive training on CQC regulations and standards to ensure their understanding and compliance with the CQC expectations. Businesses should conduct routine training sessions for staff and make sure that all team members are acquainted with the CQC policies and procedures.
Step 5: Collecting feedback from the patients and the public
Patient feedback holds significant weight with the CQC. So, to understand the services better, the healthcare business should engage with their patients and the public as this will not only reveal areas that require improvement but also showcase the business’s responsiveness to patient needs.
What if you haven’t registered your clinic with the CQC?
Healthcare practices in England or anyone who provides medical treatments, personal care, nursing care, or maternity and midwifery services, are required to sign up with the CQC, otherwise, they are committing a criminal offense.
How can practice management software help you prepare for a CQC inspection
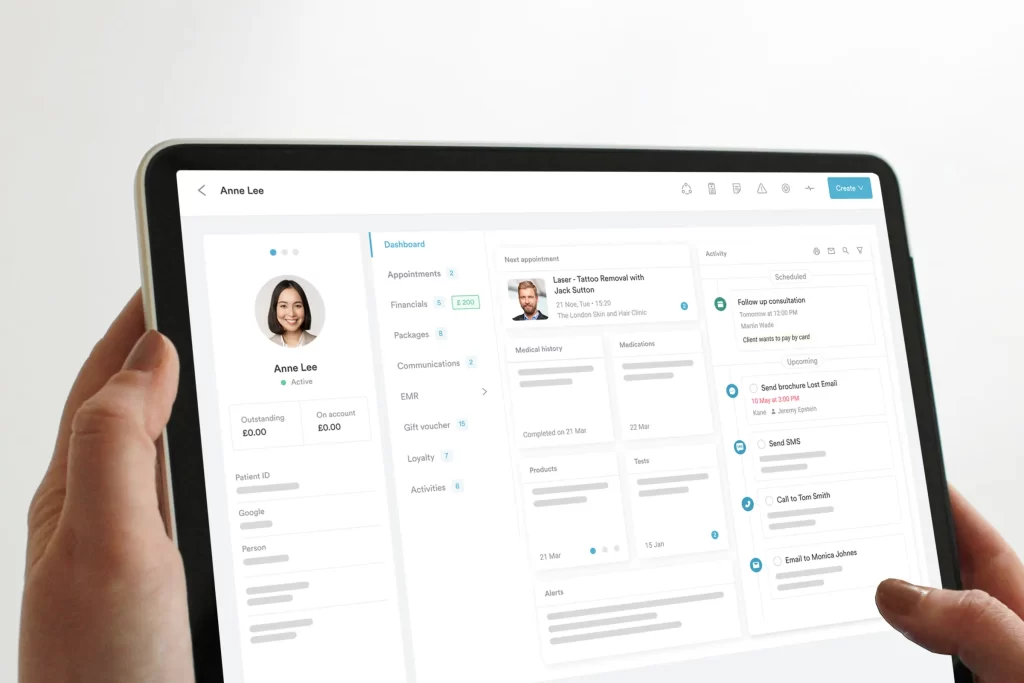
Here are just some of the ways that a robust practice management software like Pabau can help aesthetic clinics show up well at their next CQC inspection…
Extract data out of the system with only a few clicks
Creating internal audits can be a time-consuming process. But not with practice management software. Pabau lets you create automated, customizable reports on everything that goes through your practice, like staff performance, performed treatments, etc.
Collecting reviews and feedback
With practice management software, you can send automated reminders to patients to leave you reviews or give you detailed feedback after their appointments. This will help you reveal areas in your practice that require improvement and will also show that the practice is responsive to patient needs.
Having staff profiles
In the system, you will keep all your staff information and their emergency contact, keep track of their schedules and rotas, and their scheduled leave and holidays.
Having digital client records
You will have easy access to important client information, treatment notes, client photos, their medical conditions and allergies, and any other registered documentation about their treatment history. This will help you provide person-centered care, which is one of the CQC fundamental standards.
Automatically obtaining consent forms
When we are at the CQC fundamental standards, obtaining consent is one of them. With Pabau, this process will be easier than ever, as your patients will receive them right after your client books an appointment.
These are only a few aspects where practice management software can help you when preparing for a CQC inspection. Check our page to see what Pabau is capable of.
Understanding the Care Quality Commission (CQC) — Conclusion
The Care Quality Commission (CQC) serves as the pivotal regulatory body for health and social care services in England. Its primary function is to ensure that registered providers maintain high standards of safety, effectiveness, and compassion in service delivery.
The CQC operates by evaluating, inspecting, and regulating various healthcare organizations to guarantee compliance with fundamental standards, protect patients, and oversee quality.
By adhering to CQC regulations, healthcare businesses not only secure legal compliance but also secure patient safety, staff satisfaction, and overall service quality.
The CQC’s role in sharing inspection reports helps the public make informed decisions when seeking healthcare services.
Failure to register with the CQC can result in legal consequences, making compliance a crucial direction for all businesses offering medical and care services in England.
In summary, compliance with CQC regulations and standards is vital for health and social care businesses. It ensures the delivery of high-quality care, mitigates legal risks, uplifts the business’s reputation, and improves staff satisfaction.