As private healthcare becomes increasingly popular in the UK, more patients are choosing to see private GPs for faster appointments and more personalised care.
But one common question often comes up: Can a private GP refer you to an NHS specialist?
As a healthcare professional, it’s crucial to understand how private GP referrals to NHS specialists work.
When you know the process, it’s easier to coordinate care, cut down on delays, and make sure your patients move smoothly between private and NHS services.
In this guide, we’ll break down exactly how private GP referrals to NHS specialists work, and what you need to know before booking your next appointment.
How private GP referrals to NHS specialists work
In the UK, access to most NHS specialist health services requires a referral from an NHS GP.
Even when patients choose to make a private GP appointment, they typically remain registered with their NHS GP, who holds their central medical record as an NHS patient.
While private GPs can assess, diagnose, and recommend specialist care, the referral into the NHS system usually needs to be issued by the patient’s NHS GP, through the NHS e-referral service (e-RS), which can only be used by NHS clinicians
In practice, a private GP can prepare the referral documentation, but the patient’s NHS GP must then review or re-issue the referral through NHS channels before the NHS specialist appointment can be booked.
This helps keep the patient’s record up to date and ensures their care continues smoothly within the NHS system.
The role of the NHS GP in the referral pathway
Within the UK healthcare system, NHS GPs act as gatekeepers to specialist services.
This role is designed to ensure that referrals meet the NHS criteria and that patient care remains fully documented within NHS records.
Here’s how this typically plays out:
- A private GP assesses the patient and recommends specialist treatment.
- The patient shares the private referral letter with their NHS GP.
- The NHS GP reviews or issues the referral through the NHS e-referral service in accordance with NHS policies before the specialist appointment can be booked.
This process safeguards patient care by maintaining accurate NHS records and preventing fragmented treatment.
For private hospitals, aligning with this referral pathway is key to delivering a seamless experience, fostering trust with patients, and ensuring smooth collaboration with NHS hospitals.
Benefits of coordinating between private and NHS care
When private and NHS services work together, patients gain the advantages of both systems: the efficiency and convenience of private care and the comprehensive support of the NHS for long-term or specialist clinical needs.

Source: Pabau
Faster access to key services
Private GPs can often offer shorter wait times for diagnostics and specialist consultations, helping patients access early private treatment and relief from symptoms more quickly.
This can be particularly valuable for time-sensitive concerns or when NHS waiting lists are long.
By collaborating with NHS providers, clinics can help patients transition back into NHS pathways when ongoing or complex care is required.
Continuity of care and patient safety
When private and NHS providers share information effectively, it helps keep care consistent and safe.
Coordinated records mean that key details, like diagnoses, test results, and medication history, are up to date across both systems.
This reduces the chance of duplicate tests, conflicting prescriptions, or gaps in treatment, which is especially important for patients managing chronic conditions or taking multiple medications.
In short, better coordination means safer, more joined-up care for every patient.
Avoiding unnecessary repeat tests
When private and NHS providers communicate effectively, patients avoid unnecessary repeat investigations or duplicate prescriptions.
Coordinated care makes sure test results and treatments are easily accessible across systems, improving efficiency and patient trust.
For clinic owners, establishing secure, compliant communication channels with NHS partners not only supports patient outcomes but also demonstrates a commitment to quality and transparency.
These two key values build long-term credibility in the private healthcare market.
What patients need to know before seeking a private GP referral
If you run a private clinic, it really helps to set expectations around referrals from the start.
Clear communication makes it easier to work with NHS services and keeps everything running smoothly for your patients.
Source: Pabau
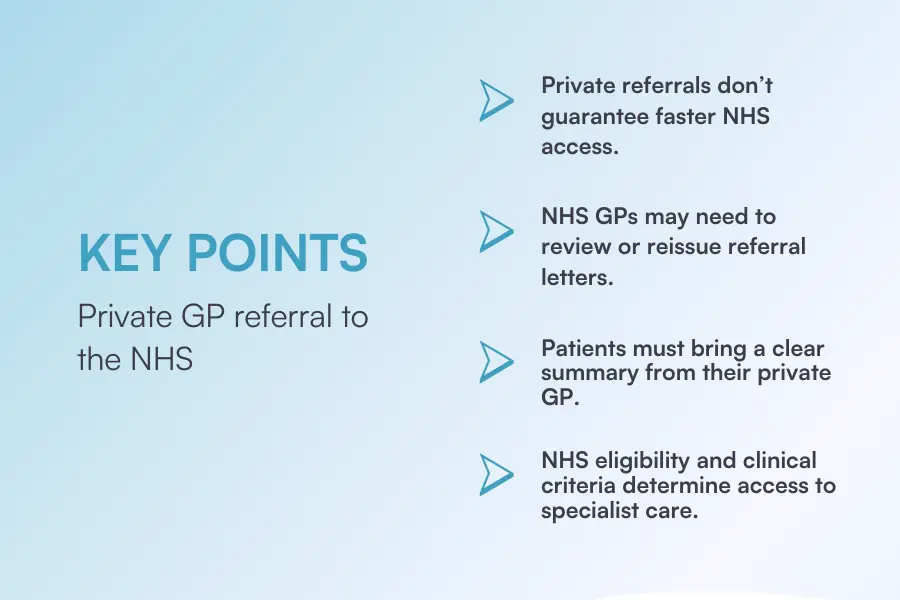
Patients often assume that a private GP referral guarantees access to an NHS specialist, but the process usually involves additional steps.
Patients should first confirm whether their NHS GP will accept and act on a private referral letter, as some may prefer to reassess the patient or issue their own referral.
It’s also best practice for patients to bring a clear summary or letter from the private GP detailing their medical issue, completed blood tests, and recommended next steps. This helps the NHS GP make an informed decision and prevents repeat investigations.
Even with private referrals, NHS eligibility and clinical criteria still apply. NHS specialists will review whether the case meets the requirements for publicly funded treatment.
How clinics can improve private to NHS workflows
Efficient coordination between private and NHS care depends on how well clinics manage data sharing, documentation, and referral communication.
Secure, compliant record systems are essential for handling sensitive patient data and ensuring smooth collaboration with NHS partners.
Every referral or shared document must meet GDPR and healthcare data standards, so having a centralized digital process reduces risks and manual errors.
Clear, standardized referral templates also help maintain professional communication and consistency when sharing information with NHS GPs or specialists.
Equally important is ensuring your team understands both NHS and private referral protocols.
Proper training ensures staff know when to escalate referrals, what documentation is required, and how to communicate effectively with NHS partners.
Leveraging technology for coordination
Technology plays a central role in improving how clinics manage referrals between private and NHS care.
Integrated systems make it easier to access patient histories, test results, and referral notes, ensuring nothing is missed and that care transitions are properly documented.
Automation can also make a significant difference. By reducing the amount of manual data entry and document handling, clinics can minimize administrative workload, prevent misplaced paperwork, and improve accuracy.
Real-time tracking of referral statuses helps staff monitor progress, follow up efficiently, and keep patients informed throughout the process.
All-in-one practice management systems like Pabau are designed with these needs in mind. It provides a centralized and compliant way to manage every stage of referral communication in one place.
The Letters feature allows clinics to send and store formal letters to GPs, specialists, or partners, while keeping a clear record of referral activity tied to each patient file.
An upcoming Client Referrals feature will also make it possible to log referrals received from other healthcare sources, giving clinics full visibility of a patient’s journey.
These tools support accurate record keeping, consistent communication, and better coordination with NHS and private partners, all key elements in maintaining high standards of care.
Common misunderstandings about GP referrals
One common misconception is that a private GP referral automatically speeds up access to NHS specialists.
In reality, NHS waiting times are based on medical need and local capacity, not on whether a patient was seen privately beforehand.
The referral may include helpful clinical details, but it won’t move the patient ahead in the NHS queue.
Another frequent misunderstanding is that patients must leave their NHS GP when using private healthcare services.
This isn’t the case since patients can remain fully registered with their NHS GP while also accessing private care.
The NHS GP continues to manage their overall health record and can coordinate with private providers as needed to ensure continuity of care.
Plus, it’s important to remember that NHS funding rules apply regardless of how the referral originated. Even if a private GP recommends NHS treatment, eligibility for NHS-funded services still depends on the usual NHS criteria and approval processes.
Foster seamless care across private and NHS services
Delivering seamless care between private and NHS services depends on clear communication, secure data management, and well-structured referral processes.
That’s where Pabau can make a real difference.
Pabau is an all-in-one practice management system designed to help clinics streamline every aspect of patient care, from booking and documentation to referrals and record sharing.
With tools built specifically for healthcare teams, clinics can:
- Track incoming and outgoing referrals in one secure system
- Communicate with GPs, specialists, and partners using branded, compliant letter templates
- Stay GDPR compliant with secure audit trails and patient data access logs
- Automate admin tasks
- Improve collaboration between private and NHS services for better patient continuity
By bringing these workflows together, Pabau helps clinics reduce administrative pressure while improving coordination, communication, and care quality across both sectors.
Discover how Pabau can help your clinic streamline referral management, secure record sharing, and reduce admin burden — book a demo today.