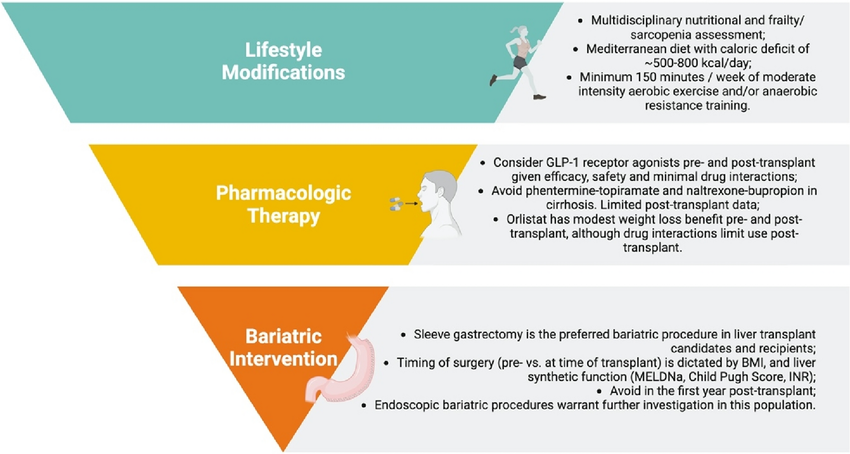
Managing metabolic health often requires a careful balance between lifestyle changes and pharmacologic interventions.
This guide explores how clinicians can evaluate, combine, and prioritize these approaches to support sustainable, patient-centered outcomes.
Understanding the foundations of metabolic health
Metabolic health management often requires a delicate balance between lifestyle interventions and pharmacologic treatments.
For clinicians, the challenge lies in identifying when behavior-based approaches suffice and when pharmacotherapy should be introduced to enhance outcomes.
Evidence increasingly supports an integrated model, where both methods are used strategically to optimize patient adherence, minimize side effects, and achieve sustainable metabolic improvements.
Lifestyle interventions: The cornerstone of metabolic care
Lifestyle modification remains the first-line therapy for most metabolic conditions, including type 2 diabetes, hypertension, and dyslipidemia. These interventions address the root causes of metabolic dysfunction, including insulin resistance, inflammation, and excess adiposity.
| Component | Clinical Focus | Typical Outcome | Adherence Rate |
|---|---|---|---|
| Nutrition Therapy | Caloric deficit, macronutrient balance, Mediterranean-style diets | 5–10% weight loss over 6 months | ~60% |
| Physical Activity | 150–300 min/week of moderate-intensity exercise | Improved insulin sensitivity, BP reduction | ~50% |
| Behavioral Therapy | Motivational interviewing, CBT, goal tracking | Enhanced adherence and maintenance | ~70% |
| Sleep Optimization | Improving sleep quality and duration | Reduced cortisol and appetite dysregulation | ~65% |
Clinical evidence consistently demonstrates that structured lifestyle programs can reduce HbA1c by 0.6% to 1.8%, decrease systolic blood pressure by 5–15 mmHg, and lower LDL by 10–35 mg/dL without medication.
These effects rival those achieved through first-line pharmacologic interventions in early-stage disease.
Pharmacologic interventions: when and why to introduce them
Pharmacologic therapies serve as essential adjuncts when lifestyle measures alone fail to achieve metabolic targets. The decision to initiate pharmacotherapy depends on disease severity, patient adherence potential, and comorbid risks.
| Drug Class | Primary Mechanism | Clinical Indication | Key Considerations |
|---|---|---|---|
| GLP-1 Receptor Agonists | Enhance insulin secretion, reduce appetite | Obesity, type 2 diabetes | GI side effects, cost, injection adherence |
| SGLT2 Inhibitors | Increase renal glucose excretion | Diabetes, heart failure, CKD | Genital infections, dehydration risk |
| Metformin | Decreases hepatic glucose production | Prediabetes, diabetes | GI intolerance, vitamin B12 deficiency |
| Statins | Reduce hepatic cholesterol synthesis | Dyslipidemia | Muscle aches, liver enzyme elevation |
Comparing lifestyle vs pharmacologic outcomes
In randomized trials, lifestyle interventions yield broader systemic benefits, while pharmacologic interventions provide targeted biochemical improvements. The most successful treatment models combine both approaches.
| Parameter | Lifestyle Interventions | Pharmacologic Interventions |
|---|---|---|
| Primary Target | Behavioral and metabolic root causes | Specific biochemical pathways |
| Time to Effect | Gradual (weeks to months) | Rapid (days to weeks) |
| Adherence | Variable, depends on motivation | High if monitored, declines without follow-up |
| Cost | Low to moderate | Moderate to high |
| Relapse Risk | Moderate, mitigated by support | High if lifestyle not maintained |
Integrative clinical approach
Modern metabolic health management emphasizes a staged, personalized approach. Clinicians should implement structured behavior change programs before pharmacologic escalation.
However, combination therapy may be warranted for patients with high baseline HbA1c (>8.5%), obesity (BMI >35 kg/m²), or multiple comorbidities.
In reproductive health, a similar principle applies: baseline hormone testing such as AMH levels interpretation gives clinicians data to personalise interventions before escalating to pharmacologic options.
Did you know?
According to a study, individuals at high risk for type 2 diabetes who lost a moderate amount of weight through one year of lifestyle counseling in primary care experienced a sustained decrease in the likelihood of requiring medication for type 2 diabetes.
Leveraging digital tools for sustainable outcomes
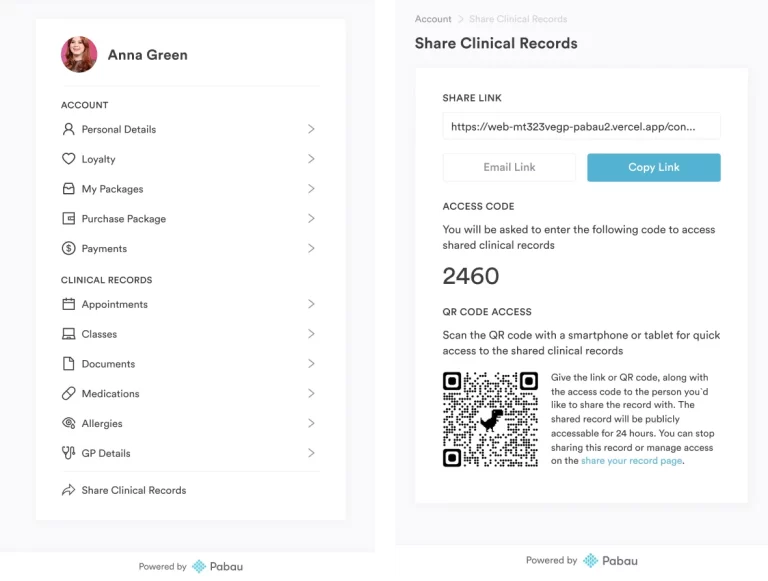
Modern clinical practice benefits greatly from digital patient management systems. Platforms like Pabau’s clinical management suite allow clinicians to track patient adherence, manage follow-ups, and ensure long-term engagement. Automated reminders and integrated health tracking can improve adherence rates by 40% or more.
Conclusion: the future is integrative
As metabolic health management continues to advance, clinicians are encouraged to adopt an integrative approach that places lifestyle interventions at the core, supported by targeted pharmacotherapy.
For patients to successfully follow this new lifestyle, ongoing support from their doctor is essential—along with timely reminders and clear instructions that are always accessible.
So, for clinics offering obesity management, diabetes care, or long-term wellness programs, Pabau provides a comprehensive solution.
Its medical-grade, all-in-one platform streamlines patient management, scheduling, documentation, and reporting—eliminating the need for multiple systems and allowing your team to focus on delivering better care.
Book a demo with Pabau today to see how it can enhance your practice and support both clinicians and patients.
References
- Lifestyle Eye Center – Lifestyle Modification
- European Journal of Cardiovascular Medicine – Evaluating the Impact of Lifestyle Interventions on Type 2 Diabetes Management
- ScienceDirect – Long-term outcomes of lifestyle intervention to prevent type 2 diabetes in people at high risk in primary health care
- ADA Guidelines – American Diabetes Association. (2025). Standards of Care in Diabetes