SOAP notes are a core part of social work documentation, providing a clear and structured way to record clinical encounters.
When written effectively, they support continuity of care, guide treatment decisions, and improve communication across care teams.
What are SOAP notes in social work?
SOAP notes are a structured method for documenting client sessions in social work and mental health.
The acronym stands for Subjective, Objective, Assessment, and Plan.
This framework ensures that every session note captures not just what a client says, but also what the clinician observes, assesses, and plans to do next.
For social workers, SOAP notes bridge empathy with accountability. They provide a clear, standardized format for recording interventions and outcomes, helping ensure consistent and legally defensible documentation.
Why SOAP notes matter in social work
In mental health settings, SOAP notes are more than administrative requirements—they are clinical tools.
Accurate SOAP documentation improves client outcomes, facilitates continuity of care, and supports multidisciplinary collaboration.
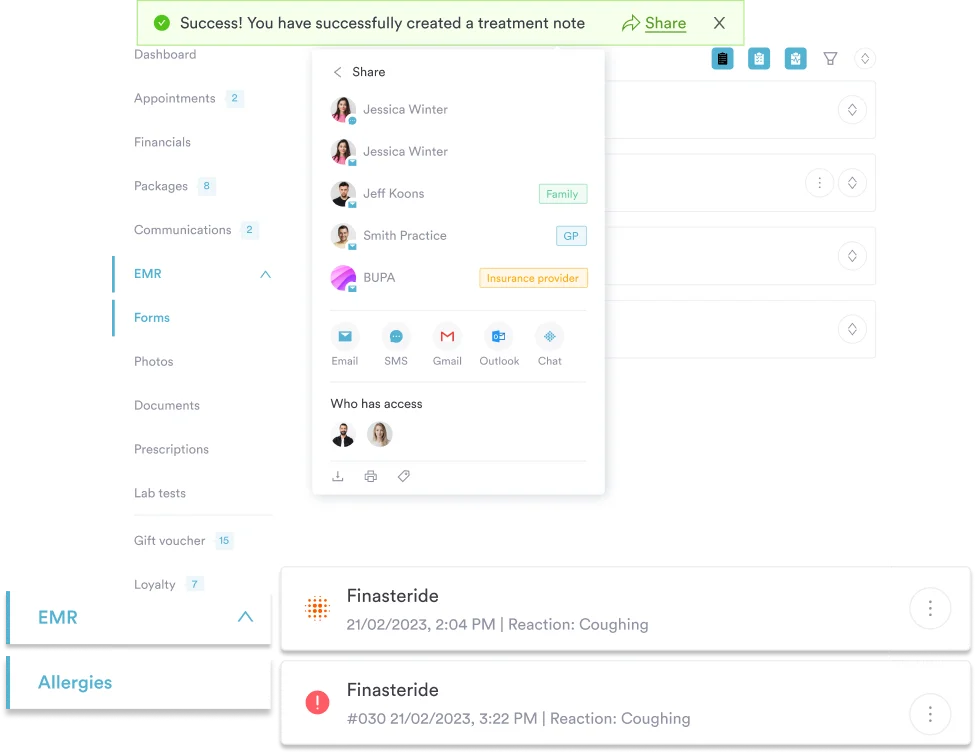
For example, if a client’s therapist, case manager, and psychiatrist all access the same record, SOAP notes allow them to see progress in a unified language.
| Benefit | Impact on Social Work Practice |
|---|---|
| Structured communication | Improves clarity between professionals |
| Accountability | Supports legal and ethical standards |
| Efficiency | Reduces time spent documenting cases |
| Continuity of care | Ensures seamless information sharing |
The SOAP framework explained
1. Subjective
This part records the client’s subjective experience—their emotions, self-reported issues, and insights.
Social workers should capture the client’s words as accurately as possible, often using direct quotes.
- Example: “Client reported feeling overwhelmed by housing instability and fears about child custody.”
2. Objective
This part covers observable facts—things you can measure or verify, such as physical presentation, attendance, or mood indicators. Here, you should stick to objective data and avoid any kind of interpretation.
- Example: “Client appeared tearful and restless during the session; speech was pressured.”
3. Assessment
The Assessment part integrates subjective and objective data.
Here, the social worker identifies patterns, progress, or risk factors and offers professional insight.
- Example: “Client’s anxiety appears linked to current financial stressors. Continues to show improvement in emotional regulation since beginning CBT sessions.”
4. Plan
The Plan outlines the next steps, including follow-ups, interventions, or referrals. It keeps the treatment goal-oriented and trackable.
- Example: “Continue biweekly sessions focusing on housing stabilization and coping strategies. Refer the client to a financial assistance program.”
Common mistakes in SOAP note writing
- Using vague language instead of measurable observations
- Blending personal opinions into the objective section
- Leaving out follow-up plans
- Failing to tie progress to treatment goals
Here are some examples of better alternatives to common mistakes:
| Common Error | Better Alternative |
|---|---|
| “Client doing better.” | “Client demonstrated improved coping by identifying three triggers for anxiety.” |
| “Session went well.” | “Client was engaged throughout session; reported decreased panic frequency from five to three times per week.” |
| “Will continue.” | “Plan to continue weekly CBT with focus on relapse prevention.” |
Did you know?
The structured SOAP format isn’t just clerical—it originated in medicine to make complex patient cases easier to understand and communicate across clinicians, and now it’s widely adopted in social work to standardise progress tracking.
Best practices for writing SOAP notes
- Write notes immediately after sessions for accuracy.
- Keep sentences concise and clinically relevant.
- Avoid jargon; use language that other professionals can interpret easily.
- Focus on behavioral evidence over assumptions.
- Always align documentation with treatment goals and ethical guidelines.
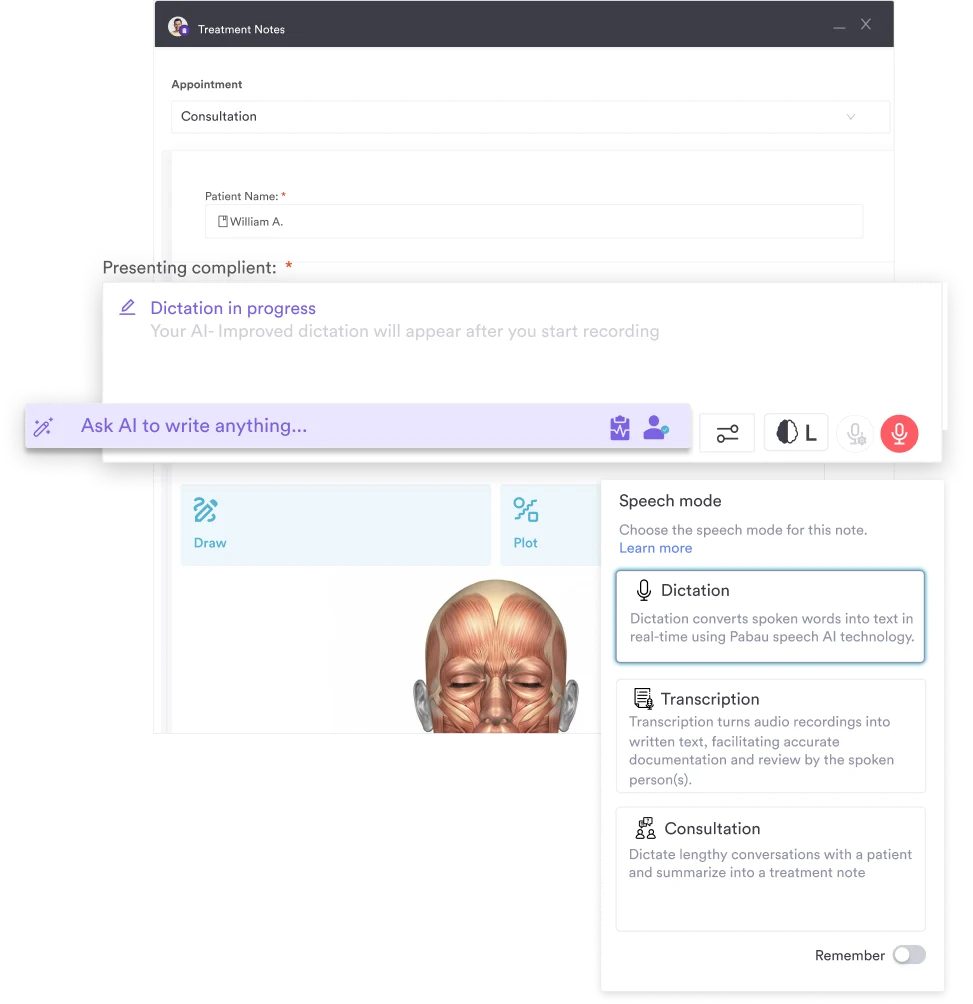
To support these practices, Pabau’s AI scribe tool can automatically capture key details during client appointments and generate structured notes, helping clinicians ensure nothing important is missed while reducing documentation time.
Integrating digital tools for SOAP notes
Modern practice management software simplifies documentation through digital templates and secure storage. These tools reduce administrative burden and improve data accessibility across teams.
With platforms like Pabau, social workers can manage digital client records, automate reminders, and standardize note formats—all while maintaining confidentiality and compliance.
Conclusion
SOAP notes remain one of the most efficient, professional, and defensible methods for documenting social work sessions. By adhering to a structured process—focusing on subjective insights, objective data, assessment synthesis, and actionable plans—social workers ensure their documentation is accurate, ethical, and client-centered.
So, if your mental health clinic manages therapy sessions, social care services, or interdisciplinary teams, Pabau can help you maintain clarity and consistency across all clinical documentation.
It offers a comprehensive, medical-grade documentation and records suite for 2026, functioning as a unified platform—so clinicians don’t need multiple systems for progress notes, follow-ups, and reports.
Request a live demo with Pabau today.
References
- Wikipedia. SOAP Notes
- Physiopedia. Soap Notes