Understanding the Role of Biomarkers in Longevity Medicine
Biomarkers are measurable biological indicators that reflect physiological processes, disease states, or responses to interventions. In the longevity field, they are used to estimate biological age, predict healthspan outcomes, and personalize interventions. However, while biomarkers have tremendous potential, their interpretation must be grounded in rigorous scientific reasoning and clinical context.
Common examples of longevity biomarkers include inflammatory markers (such as CRP and IL-6), lipid and metabolic profiles, DNA methylation clocks, and telomere length. Each of these represents a piece of a larger puzzle rather than a standalone determinant of health or lifespan.
The Scientific Promise and Pitfalls of Biomarker Interpretation
The allure of biomarkers lies in their apparent objectivity—they translate complex biological states into numerical values. Yet, this objectivity can be deceptive. Variability in testing methodology, sample handling, and patient-specific confounders can lead to misinterpretation.
For instance, while a high-sensitivity C-reactive protein (hs-CRP) level may indicate systemic inflammation, it does not identify its source or chronicity. Similarly, DNA methylation clocks can estimate biological age but should not be viewed as definitive predictors of longevity.
Clinicians must avoid overpromising what biomarkers can deliver. Instead, they should communicate results as probabilities within a continuum of risk rather than as deterministic outcomes. In the context of longevity care, this scientific humility reinforces patient trust and ethical responsibility.
Framework for Responsible Biomarker Interpretation
Responsible biomarker interpretation involves combining quantitative data with qualitative clinical judgment. A structured approach may include:
- Baseline Context: Consider patient history, lifestyle, genetics, and environmental exposures.
- Methodological Consistency: Use standardized testing protocols to ensure data reliability.
- Temporal Tracking: Evaluate biomarker trends over time rather than isolated snapshots.
- Clinical Correlation: Integrate results with symptoms, physical findings, and other diagnostics.
- Evidence-Based Translation: Link interpretations to validated clinical guidelines and research.
Commonly Misinterpreted Biomarkers in Longevity
Several biomarkers often create confusion when used in longevity discussions. Below is a summary of commonly misinterpreted markers, their significance, and interpretative cautions.
| Biomarker | Clinical Use | Common Misinterpretation | Best Practice |
|---|---|---|---|
| hs-CRP | Inflammation marker | Assumed as predictor of aging speed | Contextualize with infection status and metabolic factors |
| HbA1c | Glucose metabolism | Used as sole indicator of metabolic health | Combine with fasting insulin and lipid ratios |
| Telomere length | Cellular senescence | Viewed as absolute measure of lifespan | Interpret within biological variation range |
| DNA methylation age | Epigenetic aging | Assumed to reflect true biological age | Cross-reference with multi-omic markers |
For a detailed look at how to interpret one of the most commonly requested biomarkers in reproductive medicine, see our guide to AMH levels interpretation.
Integrating Biomarkers Into Clinical Longevity Programs
To translate biomarkers into actionable insights, clinicians should design structured longevity programs that use biomarkers as part of a broader patient monitoring strategy. Key integration steps include:
- Establishing baseline biomarker panels at initial consultation.
- Scheduling follow-up assessments at consistent intervals.
- Correlating biomarker shifts with lifestyle or therapeutic interventions.
- Using visual dashboards to communicate progress clearly to patients.
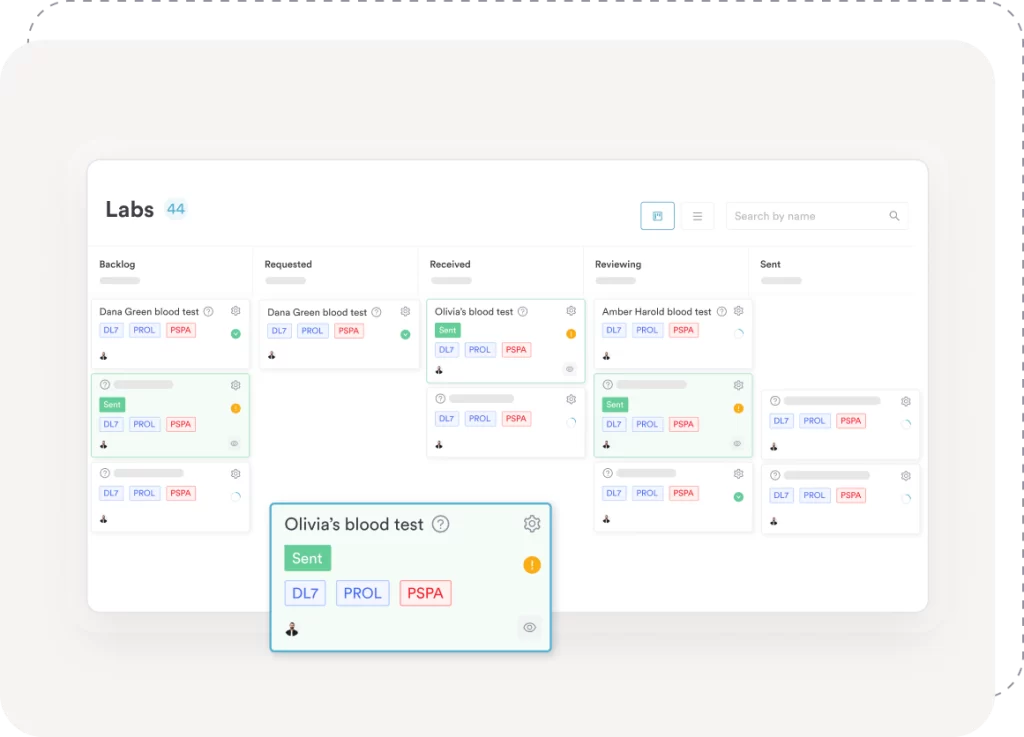
Platforms with features like Pabau’s labs feature can automate much of this workflow—collecting lab results, visualizing data over time, and supporting clinical decisions with integrated analytics.
Did you know?
Meta-analyses and methodological reviews have shown that biomarker measurements can vary substantially across laboratories and analytical methods, sometimes differing by up to ~40% for the same biomarker. This highlights the necessity for methodological consistency in biomarker testing.
Ethical Communication and Patient Expectations
One of the most critical aspects of biomarker interpretation is ethical communication. Patients seeking longevity care are often motivated by hope for extended vitality or lifespan. Overstating biomarker results can erode trust and harm clinical credibility. Instead, practitioners should:
- Use non-deterministic language (e.g., “suggests a trend toward” rather than “proves”).
- Discuss both biological variability and contextual limitations.
- Emphasize modifiable factors—nutrition, sleep, exercise, and stress—as primary levers of change.
Using integrated systems such as Pabau’s patient record helps clinicians present data visually, ensuring patients grasp the meaning of changes without misinterpretation.
From Data to Decision-Making: Closing the Loop
Ultimately, the true power of biomarkers in longevity medicine lies not in isolated numbers but in their longitudinal integration with clinical decisions. When properly interpreted, biomarkers help stratify risk, monitor interventions, and personalize patient care. However, they should never replace comprehensive assessment or clinical reasoning.
Digital health record platforms that unify lab results, patient history, and analytics—such as Pabau—empower clinicians to maintain both scientific rigor and workflow efficiency.
So, if your longevity clinic delivers precision medicine, lifestyle optimization, or advanced biomarker tracking programs, Pabau is the solution for you.
Pabau provides a medical-grade platform built around a comprehensive patient record that brings together diagnostics, lab results, patient history, engagement tools, and reporting in one place—enabling you to deliver data-driven, ethical, and transparent longevity care.
References
- AJE Advances: Research in Epidemiology (2025): Iqbal K, Intemann T, Börnhorst C, Zhang J, Aleksandrova K. Approaches for harmonization of biomarker data from multiple studies: a narrative methodological review. AJE Advances: Research in Epidemiology. 2025;1(1):uuaf005. https://academic.oup.com/ajeadvances/article/1/1/uuaf005/8131755
Request a live demo with Pabau today.