If no one followed instructions, cars would be driving the wrong way on roads, red traffic lights would be ignored, and people getting hurt would be unavoidable.
It might not always be what we want to do, but following instructions is often for the best. It’s the same with patient compliance. If patients don’t adhere to prescribed treatments, it can result in sub-optimal outcomes, worsening conditions, and increased healthcare costs.
To avoid this, understanding patient compliance is paramount.
Patient compliance is all about the extent to which patients adhere to medical advice, prescribed treatments, and recommended lifestyle changes, and it plays a pivotal role in determining the efficacy of healthcare outcomes. Let’s dive into the details.
Defining patient compliance
Patient compliance is described as a patient’s level of adherence to a given diet or treatment, as well as whether the patient returns for follow-up, re-examination, or further treatment.
In addition, patient compliance requires candor and honesty while communicating with a healthcare practitioner, so that the person caring for the patient has an accurate understanding of the patient’s condition and progress.
However, to understand patient compliance in-depth, you need to differentiate the terms compliance, adherence, and concordance.
- Compliance: How well the patient follows the practitioner’s suggestions and instructions.
- Adherence: How well the patient follows through on commitments/agreements. This involves more proactive behavior and a daily regimen — like doing physical therapy exercises.
- Concordance (or agreement): How much the patient and practitioner are aligned in their views on the treatment.
Both compliance and adherence center more on patient behavior during medication intake and lifestyle changes, whereas concordance emphasizes the underlying processes associated with medication taking. This involves building a fair and effective relationship that helps the patient during the entire course of their long-term treatment.
The significance of patient compliance in healthcare
Patient compliance is the most important factor for successful medical outcomes.
Even if the practitioner is the best one around, if patients don’t adhere to their medical routines, their treatment won’t have the desired results. And, generally, achieving adherence rates of 80% or higher is necessary for optimal effectiveness.
Patient medication compliance ensures improved health outcomes, especially for patients who need prolonged medical treatment, including:
- Patients suffering from chronic diseases
- Diabetes
- Hypertension
- Cardiovascular complications
- Different forms of cancer
- And patients who undergo aesthetic surgical intervention.
However, a staggering 50% of Americans, don’t adhere to their long-term therapy medications for chronic illnesses as prescribed.
Consequences of being patient noncompliant
The most common reason for a patient not taking a prescribed medication is: they forget.
While this sounds innocent enough, patients’ noncompliant behavior often disrupts the effectiveness of treatment for various medical conditions, and the patient’s condition might get worse and can lead to significant consequences.
Failure to adhere to medication regimens can contribute to as much as 50% of treatment failures, resulting in approximately 125,000 deaths and 25% of hospitalizations in the USA annually. In other words, patient noncompliance can have consequences both for themselves, as individuals, and for the larger healthcare system.
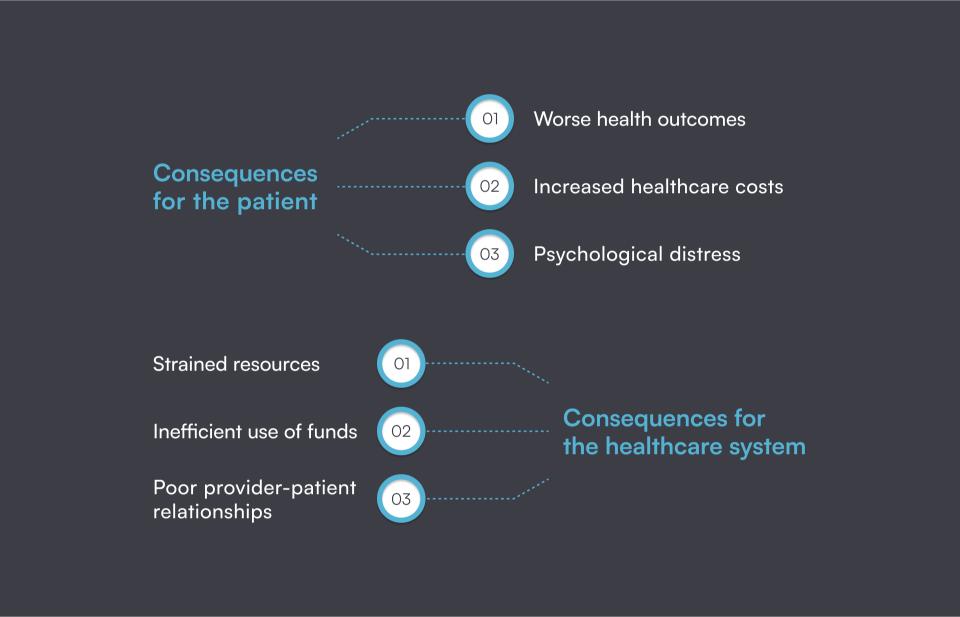
Consequences for the patient
- Worse health outcomes: Noncompliance with treatment plans can result in exacerbated symptoms, disease progression, and, in severe cases, complications or even death. For instance, skipping medications for diabetes can lead to uncontrolled blood sugar levels and potentially kidney failure. Similarly, failure to adhere to dietary recommendations after plastic surgery can significantly prolong the recovery time.
- Increased healthcare costs: Noncompliance may lead to more frequent doctor visits, hospitalizations, and emergency room interventions, increasing costs for both the patient and the healthcare system. While certain conditions may not be entirely preventable, following a physician’s guidelines significantly reduces the likelihood of requiring emergency medical care.
- Psychological distress: The guilt and anxiety associated with noncompliance can impose additional stress on the patient, which might lead to worsening their overall well-being.
Consequences for the healthcare system
- Strained resources: Noncompliance places a significant burden on healthcare professionals and resources, as patients will have to undergo more treatments than planned. This strain will also have an impact on other patients, as they might experience longer wait times and even reduced access to care.
- Inefficient use of funds: Patients who don’t adhere to physician’s treatment plans are more prone to health-related complications and require more frequent interventions. In such cases, the healthcare system spends unnecessary resources on one patient that could otherwise be used for preventive care and treatment adherence programs.
- Negative impact on provider-patient relationships: Persistent noncompliance with physician recommendations, despite repeated guidance, can lead to frustration and disappointment on the part of healthcare providers. This will potentially hinder the communication and trust between the patient and the practitioner and can lead to poor provider-patient relationships.
Factors influencing patient compliance
Patients staying compliant and adhering to medicine-taking can be a tough job, as many internal and external factors might influence it. Age, gender, education, marital status, financial status, comorbidity, duration of therapy, regime complexity, and social support are only a few factors that play pivotal roles in influencing medication adherence.
While it’s not always possible to influence all these factors, understanding why patients behave in certain ways allows healthcare providers to identify and address factors that are in their control, ultimately enhancing the likelihood of improved patient compliance.
Psychological factors
Psychological factors, such as beliefs, attitudes, and perceptions, can significantly impact an individual’s willingness to follow prescribed health plans. Positive psychological states — motivation, self-efficacy, and a strong sense of control are often associated with better adherence outcomes.
Negative emotions and poor mental health, like fear, anxiety, or depression, may lead to non-compliance, as patients may feel overwhelmed or demotivated. Feelings of shame, fear of marginalization or stigma, and uncertainty about the future can also play a role.
Factors like forgetting medication doses due to forgetfulness, changing schedules, or busy lifestyles can also contribute to non-adherence.
Furthermore, individual perceptions of illness and the perceived benefits and risk factors of treatments can shape a patient’s decision-making process, leading to intentional and unintentional poor adherence. Poor medical literacy, low treatment expectations, fear of possible side effects, and limited involvement in the treatment decision-making process are additional factors that contribute to patient noncompliance.
Understanding and addressing the psychological aspects of a patient’s experience is essential for healthcare providers in order to tailor interventions that support and enhance compliance. Building trust, providing clear information, and creating open lines of communication can positively influence a patient’s psychological state and lead to better outcomes.
Socioeconomic factors
Patients’ socioeconomic status, such as patient education levels, income, occupation, and lifestyle, correlates with patient compliance and adherence to medical treatments.
Individuals with higher socioeconomic status often have better access to healthcare resources, education, and support systems, which can contribute to their ability to adhere to prescribed treatment regimens.
On the contrary, those with lower socioeconomic status may face barriers such as limited access to healthcare facilities, financial constraints, and lower health literacy. These challenges can lead to difficulties in obtaining medications, attending follow-up appointments, and understanding complex treatment plans.
Additionally, individuals with lower social and economic status may experience higher levels of stress, which can further hinder their ability to adhere to medical recommendations. Healthcare providers should be aware of these factors and work towards implementing strategies that address the social and economic determinants of health to improve patient compliance and overall health outcomes.
Communication
Clear, empathetic provider-patient communication is key to patient compliance. It creates a strong doctor-patient relationship and enhances trust and understanding.
When physicians actively engage in discussions about treatment plans, address patient concerns, and provide comprehensive explanations, patients are more likely to comprehend the importance of adherence to prescribed therapies.
Poor communication, on the other side, such as rushed appointments or the use of complex medical jargon, can lead to misunderstandings and contribute to non-compliance.
A collaborative approach, where patients feel heard and involved in decision-making, empowers them to take an active role in their care.
Additionally, physicians who encourage patients to ask questions, actively listen to patient perspectives, and consider individual preferences contribute to a supportive environment that promotes adherence. Regular follow-up communication can also reinforce treatment plans, address emerging issues, and provide ongoing motivation.
The role of technology in enhancing patient compliance
Nowadays, our attachment to smartphones is undeniable. While the thought of taking time off for a health check-up may often feel like too much to ask in our busy schedules, we always seem find the time to scroll through a bunch of reels before bedtime.
That’s why connecting healthcare professionals and facilities to technology is crucial for boosting patient compliance. All-in-one practice management software, such as Pabau, can help healthcare organizations establish clear and timely communication with patients.
This can be achieved through:
- Automatic email and SMS reminders and client recalls — With the help of practice management software, you can nudge clients and remind them about their upcoming appointments, leading to fewer no-shows and enhanced patient compliance.
- Automatic client recalls — Through management software, you can efficiently notify clients about upcoming check-ups or follow-up treatments by setting up automatic client recalls. You can choose which treatments or services to set up and tailor them to individual client groups, ensuring a personalized and targeted approach.
- Sending pre and after-care instructions — Providing clients with educational resources on how to prepare for upcoming appointments and maintain their treatment post-visit is instrumental in reinforcing their commitment to the prescribed care plan. Rather than only telling them verbally, this means they can access treatment instructions at any time.
This minimizes the risk of the client forgetting essential details and disengaging with their treatment and fosters a greater understanding of their treatment journey.
Here’s how Pabau, the all-in-one practice management software, can help you improve the patient journey in your clinic.
- Access to patient portals — This will enable patients to access their health information, appointment history, and treatment details seamlessly via a secure website. Through the patient portal, patients can effortlessly book upcoming appointments, access documentation sent by the practitioner, review progress photos, and much more.
- Telehealth consultation — Busy schedules can interfere with patient adherence and contribute to missing crucial follow-up appointments. That’s why offering telehealth consultations that patients can attend from their homes can greatly impact patient engagement and compliance.
- Electronic client cards — Practice management software will automatically store all your clients’ information in one place, including their health and appointment history, treatment plans, and other crucial details so clinicians can easily track patients’ treatment adherence. Going paperless can save your staff time and improve efficiency in your clinic.
Learn more about the benefits of going paperless in your clinic.
Enhance patient compliance with Pabau
Paying personalized attention to each individual client with manual processes is impossible.
Imagine having to remember to notify each client about upcoming appointments or follow-up treatments. Although it may seem more impersonal, clever technology can help you create more personalized care at scale.
This is where implementing practice management software becomes a crucial step toward achieving successful patient compliance.
Pabau stands out as one of the most comprehensive all-in-one practice management software solutions, specifically designed to assist healthcare organizations in enhancing patient compliance. Leveraging Pabau’s automated features, healthcare providers can deliver personalized patient care, fostering strong patient-provider relationships.
With just a few clicks, you can effortlessly send appointment confirmations and reminders and important treatment details and monitor their progress. Additionally, Pabau aids in maintaining compliance within your healthcare organization, such as:
- Documented and easily accessible pre-care and post-care instructions
- Convenient ways to book and self-manage appointments
- Reminders for follow-up care that you can personalize to the service
Check out this HIPAA compliance checklist for medical spas.
If you want to find out all the ways Pabau can help with patient compliance, book a demo now