Checklists have a funny way of making overwhelming tasks a little bit less overwhelming.
Just like when you go to the store. If you don’t have a list of all the groceries you need to buy, you’ll either forget to buy something or overspend on things you don’t even need.
It’s the same when preparing for a CQC inspection.
Without a clear checklist to follow, you might focus on something unimportant and overlook crucial aspects that matter to the CQC inspection team.
Achieving CQC compliance takes a lot of work. And while it may feel like a lot of hoops to jump through, it’s not just a box-ticking exercise – it’s actually a way to make your general practice even better.
It’s a two-way street that leads to one mutually desired destination — ensuring better patient care.
From the very beginning — registering with the Care Quality Commission and informing your general practice for the upcoming inspection, to the day of the visit, you have to make sure you are CQC compliant. If you want to grab your checklist and go, you can.
We tell you everything in detail in this blog. So keep on reading and you’ll find everything you’ll need to know about CQC compliance.
What is the CQC (Care Quality Commission) and its role?
The CQC is England’s independent regulator of health and social care.
Through monitoring and inspections, the CQC ensures healthcare organizations meet the necessary health and social care standards in England and makes sure the services they provide to patients are of the best quality.
After the inspection, the CQC will publish the insights and performance ratings with the healthcare organization and will make the ratings available to the public.
Check out our blog and learn everything you need to know about CQC and its role.
The CQC regulates many departments, such as hospitals, dentists, and clinics, but in this blog, we’ll be focused on general practices and how they can prepare for a CQC inspection.
How the CQC monitors general practices
The CQC follows the Intelligent Monitoring dataset when inspecting GP practices.
The Intelligent Monitoring (IM) report pulls information that is available in the public domain such as patient surveys, QOF (Quality and Outcomes Framework) reports, and other information, to give the inspectors an overview of the weaknesses and strengths of the general practices they inspect, which allows them to perform more targeted inspection visits.
CQC insights
The CQC gathers insights by analyzing information about services together with national and local data in order to spot potential changes in the general practice’s quality of care.
These insights help the CQC in determining when, what, and which services to inspect.
They use the insights to compare a practice’s data with all other practices in England. The CQC evaluates the performance of the practices, which provides them with a statistical measure of a practice’s performance compared to the England average.
Then the CQC highlights the ones that significantly vary from England’s average.
How the CQC collects information about general practices
The way the CQC collects information depends on the practice’s previous ratings:
- Inadequate
- Requires improvement
- Good
- Outstanding
Practices with ratings of requires improvement or inadequate:
If your general practice gets an inadequate rating, then the CQC will inspect the practice within six months.
If your practice requires improvement, then the CQC will visit your practice for inspection within 12 months.
Practices with ratings of good and outstanding:
For practices that have outstanding or good ratings, the CQC will perform a formal regulatory review every year. The inspection team will spot any changes by reviewing:
- Information provided by the practice
- The CQC insights
- Input from collaborators, such as Clinical Commissioning Group (CCG) or Healthwatch
If the review suggests that the quality of care may have improved or declined since the last rating, the CQC may opt for an inspection, but if they don’t need to take any actions, they will:
- Inform you that the review has been conducted, and no further action is currently required
- Publish a note about this on their website
CQC registration
Before the general practice starts providing services, they must apply for CQC registration. The GP practice registration must be kept up to date and include any recent changes to the Registered Manager, Partnership, Statement of Purpose, and Regulated Activities.
As part of your application, you will have to show:
- Documentation on how you will meet the Health and Social Care Act 2008, relevant guidance, associated regulations, and other applicable laws
- Whether you’ll follow the CQC Fundamental Standards:
- Providing person-centered care
- Treating patients with dignity and respect
- Asking for consent
- Being responsible for patients’ safety
- Safeguarding from abuse
- Providing enough food and drink
- Clean premises and equipment
- Receiving and responding to complaints
- Ensuring good governance
- Have qualified, experienced, and competent staff
- Hiring fit and proper staff
- Duty of candour — being open and honest to patients, and publicly displaying ratings
- That you have well-designed plans in place and you’ll provide all the necessary documentation
- Written Care Policies and Procedures and show that the staff understands them
- That you and your staff understand what is required of you
- The location and building are appropriate for delivering care
How the CQC informs general practices of upcoming inspections
Before the inspection, general practices will receive an initial notification letter.
The CQC inspector will call the general practice to formally announce the inspection, and a confirmation letter will be sent to confirm the date and time of the inspection.
Don’t worry, this doesn’t mean that the inspection team will visit you right away. A two-week notice period will be provided ahead of the inspection.
The CQC will also send a letter to the general practice requesting specific information. The letter will explicitly outline the details of the information that is required, including where to submit it and contact details in case you have any questions.
After receiving the letter, GP practices will have five working days to respond to the letter and provide the necessary documentation.
Typically, you may be requested to provide the following documentation:
- Evidence of the monitoring of service and treatment quality. This consists of documentation from two clinical audit cycles that have been finished during the last 12 months, as well as documentation from any other audits, alongside evidence of the actions taken and the reached results.
- A summary of all complaints received throughout the last 12 months, along with any related actions taken and implemented learnings.
- A summary of all significant incidents that happened during the course of the previous 12 months, along with the actions taken and implemented learnings.
- An action plan that takes into consideration the results of any completed patient surveys.
- The number of full-time staff by role.
- Training and recruitment procedures and policies (how staff are recruited and trained before they start working, arrangements for foreign doctors, and what kind of introduction they receive.)
- General practices should also provide posters (guidelines, or other relevant details related to the GP practice) and comment cards (on which patients or individuals can provide feedback) that are supplied with the practice’s inspection letter notification.
- A copy of the current Statement of Purpose (the statement of purpose explains what you do, who you do it for, and where you do it.)
How to prepare your general practice for CQC inspection — checklist
The manager of the general practice should take responsibility for preparing all the areas of the practice for the inspection. That will include:
- Organizing and decluttering all areas within the GP practice
- Being prepared for potential questions from the CQC inspector regarding the contents of the doctor’s bag, fridge temperatures, emergency drugs, and associated logs
- Making sure that the practice has good stock control systems
Having robust practice management software that will help you with inventory management can be of big help when organizing your stock levels in your practice and won’t let you have any out-of-date stocks.
Pabau will simplify the stock management process and will automatically register any stock updates and deductions, so you’ll always know where you’re up to with your clinic’s stock levels.
4. Removing all medical and non-medical stock that is out of date, materials, and medical-related resources such as the British National Formulary (UK’s pharmaceutical reference book)
5. Making sure all the medical supplies cupboards are securely locked
6. Making sure keys are kept in a safe and secure place
7. Identifying and assessing potential hazards and risks in the area where controlled drugs are stored
8. Having trained first aider and a safe aid box in a designated area
9. Verifying the proper placement and expiration dates of all fire equipment
10. Ensuring that an incident/accident book is kept in a designated area and is available for the workforce to complete
11. Make sure to identify and maintain an isolation room, along with appropriate policies for its use
12. Having private area patients can use, including a breastfeeding room where possible
13. Make sure you are ‘zoning’ information — bringing information together in specific zones and displaying them within the general practice and on the business’ website to help with CQC compliance. This might include information like how consent is obtained from patients, which services are offered at the GP practice, how confidentiality is ensured, etc.
14. Having a place for patients to leave both positive and negative feedback and complain about the services and care they received
15. Ensuring you have displayed information about the Patient Participation Group (PPG is a group made up of GP practice staff, carers of registered patients, and GP practice patients aged 16 years and over.)
Documentation needed when the CQC inspection arrives in your general practice — checklist
On the day of the inspection, the CQC inspection team will meet with the general practice manager or a senior member of the GP. The Chief Inspector will explain the purpose of the inspection and who the inspection team is.
After the introduction and before the inspection starts, the inspector will ask for the documentation they need from the general practice.
Practices should have these key documentation on hand:
- Records of significant events
- Audits covering cleanliness, infection control, and disability access
- Documentation about risk assessments, and evidence that reasonable actions were taken
- Documentation for health and safety
- Business continuity plan
- Human resources policies, staff files, and procedures, including induction programs and a Locum Policy
- Operational policies for services, including complaints, safeguarding, medicine management, chaperoning, and repeat prescribing
- Reports on equipment calibration
- Portable Appliance Testing (PAT) reports
- Registers for palliative care
- Workforce schedules and training matrix
How to present your general practice in the best light for the CQC inspection
Prepare for the 30-minute presentation
After the inspection team arrives in the general practice and introduces themselves, it’s time for the GP’s manager or senior member of staff to give a presentation to the inspection team.
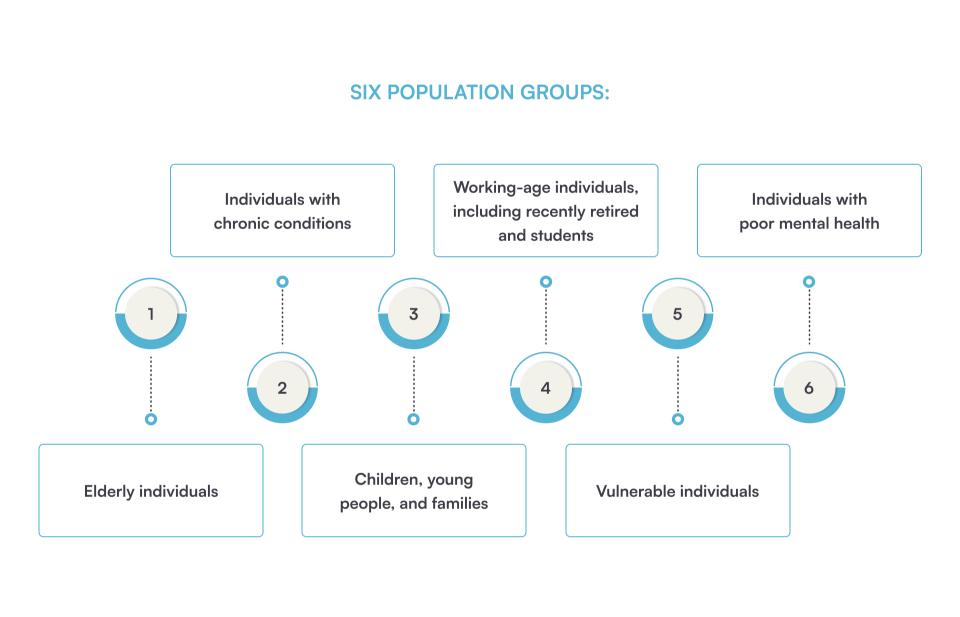
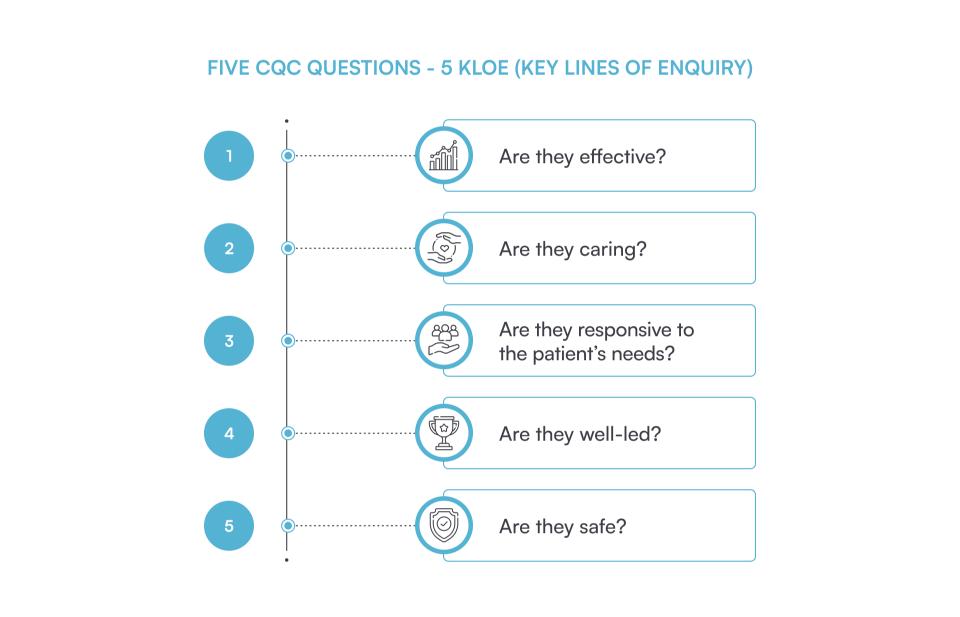
The presentation should last for around 30 minutes and should be about the GP’s own view of their performance, specifically in relation to the six population groups and five CQC questions.
With this presentation, you create the first impression, so it’s important to prepare for it as much as possible.
Things to cover in the presentation
The best thing you can do during this presentation is to highlight everything about your practice openly. So besides highlighting the strengths of the practice, you should also use this presentation to be open about the risks and challenges the general practice faces.
- You can start by highlighting the cultural characteristics and a bit of history of the general practice.
- Explain how the general practice works, covering things like how you choose the staff and what you do to keep them, how many patients they have, the different groups of people they help, and the general characteristics of the patients.
- Discuss the CQC Intelligent Monitoring dataset of the practice and explain why your practice may show up on particular indicators, whether you believe it poses a risk, and what, if any, actions have been taken.
- Present how the general practice is well-led by showing how you improve quality by conducting staff trainings, listening and responding to patient’s complaints, and how your practice overcomes challenges and threats.
- Outline all the services that have been improved.
- Show what kind of access you have to all of the appointments and services.
- Identify the strong sides of your practice in each of the five key questions.
- Give examples of how you provide outstanding care.
- Go through your care plans and show how the practice collaborates with other organizations and professionals.
- Discuss some specific patient cases (anonymously) with the inspection team to demonstrate compliance.
- Include reviews and feedback from patients to show them that you care for patient’s opinions.
- Share an example where a staff member went the ‘extra mile’ to achieve the best possible outcome for patients.
- Discuss what you and your staff are doing to improve the areas in your general practice that are not so good.
- Present the practice’s clinical and non-clinical audit cycles, and discuss what you’ve learned and which areas need change.
Other tips on how to prepare for the inspection
- Make sure that you can access all the general practice’s information quickly — robust practice manager software can help you with this as you’ll have all the information about your patients, staff, and other data in one system.
- The CQC Inspector will probably ask you to show them the appointment availability to access GPs and nurses, and how you book services in advance and those that are urgent. That’s why you should make sure that the booking system you have is advanced to meet all the needs of the general practice.
- Make sure that you have a website for your practice and keep it up-to-date.
- Make sure your most experienced staff is working on the day of the inspection.
- Display previous CQC ratings where are most visible.
- Make sure the equipment and the premises are properly used, clean, and sanitised, and ensure a hand gel is available in key areas.
Taylor Wilson — Certified Recovery Specialist
Taylor has worked in the recovery field since 2013 and has been a recovery coach since 2015. He's also a founder of Active Recovery Comapnions.
“When the CQC inspection team arrives, there is typically an initial meeting where they introduce themselves and explain the purpose of the inspection. They will ask for relevant documentation, such as policies and procedures, staff qualifications and training records, and patient feedback.
“Communication with practitioners and patients is a key aspect of the inspection. The CQC inspectors will conduct interviews and discussions with the practitioners to get an understanding of how the practice operates. They may ask about patient care, infection control measures, safeguarding procedures, and other aspects of service delivery.
“In my experience, the CQC inspectors pay close attention to several areas during the inspection. They thoroughly review patient records and documentation to ensure compliance with standards. They also closely examine cleanliness and infection control practices, as well as the staff’s knowledge and adherence to protocols.
“Patient feedback, both positive and negative, is taken into account as well.
“Overall, the CQC inspection process aims to assess the safety, effectiveness, and quality of care provided by healthcare practices. It is a comprehensive evaluation that covers various aspects of the practice’s operations.
Read our blog and learn how to respond to bad patient feedback the right way.
Practice management software can make it easier for you to prepare for the CQC inspection
If you use practice management software in your practice, one with robust features such as the practice management software Pabau has, you’ll have all the information securely stored in one system.
- You’ll have workforce schedules built into the system and you can plan ahead, create repeatable schedules, and block time out for staff training or leave.
- You’ll have a built-in system for feedback which enables you to automatically request feedback after every appointment and make it specific to the service.
- The software will also help you with gathering important data, as it can generate automatic reports and give you an overview of the targets you’ve set and the ones you achieved.
- Within the software, you can also manage all your inventory as it updates new and deducts used items automatically.
And many other helpful features.
Understanding the Care Quality Commission for general practices
In summary, preparing for the CQC inspection is crucial for the success and reputation of general practices in England. General practices need to be well-prepared for the inspection, starting with the initial CQC registration and extending to the day of the inspection.
When preparing for a CQC inspection, you need to follow a comprehensive checklist so you can adhere to CQC compliance. This checklist involves organizational and business skills, decluttering efforts, good stock management, paying attention to details, and much more.
General practices should also be ready to present their strengths, challenges, and improvements during the visit.
While the inspection process, in some cases, can be rigorous, the use of practice management software, such as Pabau, can streamline data management, scheduling, reporting, and more.
By following best practices and staying compliant with CQC standards, general practices can not only ensure the delivery of quality care but also maintain positive CQC ratings.



